Ozone and Your Patients' Health
Health Effects of Ozone in the General Population
| Review Key Points |
- Introduction
- How are people exposed to ozone?
- How does ozone react in the respiratory tract?
- What are ozone's acute physiological and symptom effects?
- What effects does ozone have at the cellular level?
- How does response vary among individuals?
- What are the effects of ozone on mortality?
- What are other effects of short-term ozone exposure
- What are the effects of recurrent or long-term exposure to ozone?
- At what exposure levels are effects observed?
Introduction
Inhaling ground-level ozone can result in a number of health effects that are observed in broad segments of the population. Some of these effects include:
- Induction of respiratory symptoms
- Decrements in lung function
- Inflammation of airways
Respiratory symptoms can include:
- Coughing
- Throat irritation
- Pain, burning, or discomfort in the chest when taking a deep breath
- Chest tightness, wheezing, or shortness of breath
In addition to these effects, epidemiologic evidence strongly indicates that higher daily ozone concentrations are associated with increased asthma attacks, increased hospital admissions, increased daily mortality, and other markers of morbidity.
This first section addresses exposure and health effects issues common to all people. The following section addresses those issues specific to people with asthma, a group especially susceptible to ozone, and possibly people with other existing lung diseases.
How are people exposed to ozone?
Exposure occurs when people inhale ambient air containing ozone. The rate of exposure for a given individual is related to the concentration of ozone in the surrounding air and the amount of air the individual is breathing per minute (minute ventilation). The cumulative amount of exposure is a function of both the rate and duration of exposure.
Although ozone concentrations in the outside (ambient) air are generally similar across many locations in a particular airshed, a number of factors can affect ozone concentration in "microenvironments" within the larger airshed (e.g., inside a residence, inside a vehicle, along a roadway). Ozone concentrations indoors typically vary between 20% and 80% of outdoor levels depending upon whether windows are open or closed, air conditioning is used, or other factors. People with the greatest cumulative exposure are those heavily exercising outdoors for long periods of time when ozone concentrations are high. In addition, during exercise people breathe more deeply, and ozone uptake may shift from the upper airways to deeper areas of the respiratory tract, increasing the possibility of adverse health effects. People with the lowest cumulative exposure are those resting for most of the day in an air-conditioned building with little air turnover.
Outdoor ozone levels may also affect indoor levels of some aldehydes formed as reaction products of ozone with indoor substances (Apte et al 2008). This provides a potential pathway for people indoors to experience respiratory effects mediated by ozone reaction products. Further research is needed to test the importance of these exposures on health effects.
How does ozone react in the respiratory tract?
Because ozone has limited solubility in water, the upper respiratory tract is not as effective in scrubbing ozone from inhaled air as it is for more water soluble pollutants such as sulfur dioxide (SO2) or chlorine gas (Cl2). Consequently, the majority of inhaled ozone reaches the lower respiratory tract and dissolves in the thin layer of epithelial lining fluid (ELF) throughout the conducting airways of the lung.
In the lungs, ozone reacts rapidly with a number of biomolecules, particularly those containing thiol or amine groups or unsaturated carbon-carbon bonds. These reactions and their products are poorly characterized, but it is thought that the ultimate effects of ozone exposure are mediated by free radicals and other oxidant species in the ELF that then react with underlying epithelial cells, with immune cells, and with neural receptors in the airway wall. In some cases, ozone itself may react directly with these structures. Several effects with distinct mechanisms occur simultaneously following a short-term ozone exposure and will be described below.
What are ozone's acute physiological and symptom effects?
Controlled human exposure studies have demonstrated that short-term ozone exposure - up to 8 hours - induces lung function decrements such as reductions in forced expiratory volume in one second (FEV1) and the following respiratory symptoms:
- Cough
- Pain on deep inspiration
- Shortness of breath
These effects are reversible, with improvement and recovery to baseline varying from a few hours to 24 to 48 hours after an elevated ozone exposure.
Current thinking is that both symptom and lung function changes are due to stimulation of airway neural receptors (probably airway C-fibers) and transmission to the central nervous system via afferent vagal nerve pathways. Although ozone exposure results in some airway narrowing, neural inhibition of inspiratory effort at high lung volumes is believed to be the primary cause of the predominant physiological effect, being unable to inhale to total lung capacity (TLC).
The overall effect is thus primarily restrictive in nature with a smaller obstructive component and reflects itself in decreases in forced vital capacity (FVC), FEV1 and other spirometric measures that require a full inspiration. It is likely that these lung function changes and respiratory symptoms are responsible for observations that short-term ozone exposure limits maximal exercise capability.
Ozone-induced changes in breathing pattern to more rapid shallow breathing may also be a manifestation of C-fiber stimulation and may be a protective response to limit penetration of ozone deep into the respiratory tract. Such effects may also contribute to changes in deposition pattern and retention of other inhaled substances such as allergens and particulate air pollution.
What effects does ozone have at the cellular level?
As a result of short-term exposure, ozone and/or its reactive intermediates cause injury to airway epithelial cells followed by a cascade of other effects. These effects can be measured by a technique known as bronchoalveolar lavage (BAL), in which samples of ELF are collected during bronchoscopy on volunteers experimentally exposed to ozone. Cells and biochemical markers in the lavage fluid and in the blood can be analyzed to provide insight into the effects of exposure.

Evidence for airway inflammation following ozone exposure includes visible redness of the airway seen during bronchoscopy as well as an increase in the numbers of neutrophils in the lavage fluid. Cellular injury is suggested by an increase in the concentration of lactate dehydrogenase (LDH), an enzyme released from the cytoplasm of injured epithelial cells, in the ELF. Mediators (e.g., cytokines, prostaglandins, leukotrienes) that are released by injured cells include a number that attract inflammatory cells resulting in a neutrophilic inflammatory response in the airway. In addition, ozone reaction products as well as some mediators produced in the lung can be detected in the blood providing a possible mechanism for extrapulmonary effects of ozone exposure.
Other effects that may be related to the underlying injury and inflammatory response are:
- An increase in small airway obstruction
- A decrease in the integrity of the airway epithelium
- An increase in nonspecific airway reactivity
The decrease in epithelial integrity can be measured by an increase in the concentration of plasma proteins appearing in the ELF following exposure and by more rapid clearance of inhaled radio-labeled markers from the lung to the blood. This has the potential for allowing increased movement of inhaled substances (e.g. allergens or particulate air pollution) from the airway to the interstitium or the blood and could modify the known effects of inhaled allergen on asthma and particulate matter on mortality.
Although the significance of increased nonspecific airway reactivity to substances such as methacholine or histamine is not understood in healthy individuals, it is clearly of concern for people with asthma, as increased airway reactivity is a predictor for asthma exacerbations. (See section entitled How does ozone affect people with asthma?).
Over a period of several days following a single short-term exposure, inflammation, small airway obstruction, and increased epithelial permeability resolve; damaged ciliated airway epithelial cells are replaced by underlying cells; and damaged type I alveolar epithelial cells are replaced by more ozone-resistant type II cells. Over a period of weeks, the type II cells differentiate into type I cells, and following this single exposure, the airway appears to return to the pre-exposure state.
How does response vary among individuals?
One striking characteristic of the acute responses to short-term ozone exposure is the large amount of variability that exists among individuals. For example, for a 2-hour exposure to 0.4 parts per million (ppm) ozone that includes 1 hour of heavy exercise, the least responsive individual may experience no symptom or lung function changes while the most responsive individual may experience a 50% decrement in FEV1 and have severe coughing, shortness of breath, or pain on deep inspiration. A similar range of response is evident for a 6.6-hour exposure to 0.08 ppm with 5 hours of moderate exercise. Other individual responses fall into what appears to be a unimodal distribution between these two extremes. Those with large (small) responses following exposure on one day also tend to have large (small) responses upon re-exposure. A small fraction of the observed variability in lung function and symptom responsiveness can be explained by differences in age and in body mass index (BMI) with young adults (teens to thirties) and those with high BMI being much more responsive than older adults (fifties to eighties) and those with low BMI. Results similar to those in Figure 7 are also seen with longer duration exposures to concentrations more relevant to ambient levels (e.g. over a range of 0 to 0.12 ppm).
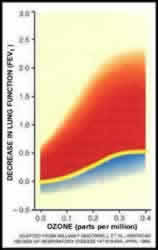 Figure 6: Variability of
response to ozone exposure. Figure 6: Variability of
response to ozone exposure. Source: Devlin et al. (1997) |
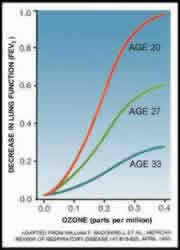 Figure 7: Sensitivity to ozone exposure
is age related. Figure 7: Sensitivity to ozone exposure
is age related. Source: Devlin et al. (1997) |
|
|
Individual differences in the intensity of the inflammatory response also exist, and it appears that these differences in response are also stable over time. The magnitude of the neurally-mediated lung function response, however, is not related to the degree of cell injury and inflammation for a given individual suggesting that these two effects are the result of different mechanisms of action. Further evidence for multiple mechanisms of action is provided by drug intervention studies. There is some evidence that Vitamin C and E supplementation may slightly reduce the lung function effects of ozone but not the inflammatory or symptom responses. Pre-treatment with non-steroidal anti-inflammatory drugs (NSAID) reduces lung function and symptom responses but not the inflammatory responses in non-asthmatics. In asthmatic volunteers NSAID pretreatment did not block the restrictive lung function changes seen in nonasthmatics, but did blunt some of the changes due to airway obstruction. Pre-treatment with high doses of inhaled steroids has been shown to reduce the neutrophil influx following ozone exposure in asthmatic volunteers, but not in those without asthma.
True differences in individual responsiveness to ozone can be the result of either environmental or genetic factors. Research has demonstrated that genetic differences among strains of mice can explain the large range of inflammatory responses seen among these strains. Some preliminary evidence suggests that genetic polymorphisms for antioxidant enzymes and for genes regulating the inflammatory response may modulate the effect of ozone exposure on pulmonary function and airway inflammation.
What are the effects of ozone on mortality?
Recent epidemiologic research has clearly demonstrated that both short-term and longer-term exposures to low concentrations of particulate matter, a common air pollutant, are associated with increased mortality. Re-examination of the data upon which those findings are based as well as new studies indicate that short-term exposure to ozone is also associated with increased daily mortality. The study most representative of the U.S. population (Bell et al 2004) evaluated the relationships between daily mortality counts and ambient ozone concentration for 95 large U.S. communities over the period of 1987-2000. Although there was considerable heterogeneity in the magnitude of effect among the various communities, a 0.5 % overall excess risk in non-accidental daily mortality was observed for each 20 ppb increase in the 24-h average ozone concentration (approximately equal to a 30 ppb increase in the 8-h average) on the same day. There was evidence that the effect was greatest on the day of exposure with smaller residual effects being evident for several days. A cumulative 1.04% excess risk was observed for each 20 ppb increase in the 24-h average concentration during the previous week. The ozone-mortality relationship was robust even after controlling for possible effects of particulate matter and other air pollutants.
Choose between the following 2 versions and delete the one you don’t want to use (I am trying to make 2 points here. First about older individuals having a larger absolute effect even with a similar relative risk and second that for a given individual on a single day the risk is not high).
[1. To put these risk estimates in perspective, a 35 year old female with an average life expectancy of 51 years has a 3.942 x 10-6 probability of dying on a given day. An increase of 0.5% would increase the probability to 3.962 x 10-6, a small absolute increase in risk For a 75 year old male with a life expectancy of 10 years, a similar percentage increase would increase the probability from 1.176 x 10-4 to 1.182 x 10-4. Although the absolute increase in risk of dying on a given day is much higher for the older individual because the baseline risk is higher, it is still quite small for a given individual. On the other hand, because of the large number of individuals at risk across the country, an effect of this magnitude has meaningful public health implications.]
[2. Although ozone mortality risk estimates tend to be only slightly higher for the older (>65 years) population compared to the younger population, the absolute effect of ozone on mortality is considerably higher in the elderly due to their higher baseline death rates. Even for the elderly, however, the risk of dying on any given day as a result of ozone exposure is quite small. On the other hand, because of the large number of individuals at risk across the country, an effect of this magnitude has meaningful public health implications.]
A preponderance of other time series studies supports the existence of an ozone-mortality relationship although with a wider range of effect estimates primarily due to the smaller sizes of the studies. An independent review of this literature by the National Research Council concludes that short-term ozone is likely to be associated with premature mortality.
Other observations made in these studies include the finding that the ozone-mortality relationship is most prominent during the warm season, with few or smaller effects in the winter. It also appears that the ozone-mortality association persists when deaths are limited to those caused by either cardiac or pulmonary disease or to those caused by cardiovascular disease alone. Risk estimates for other causes of death are generally inconsistent across studies probably reflecting the lower statistical power associated with smaller daily death rates. In the Bell study of 95 cities, the observed city specific effect rates varied widely. The degree to which this variability reflects different ozone-mortality relationships in the different cities is not clear, but it does raise the question as to whether a single average 0.5% increase in daily mortality rates should be applied to all cities. Other unanswered questions pertain to the lowest concentrations at which these effects occur and the possible mechanisms of action responsible for increased mortality among many who spend much of their time indoors where ozone levels are generally quite low. Bell et al. divided days into those with a 24-h average ozone concentration above and below 60 ppb and found that the relationship was similar for both subsets suggesting that the relationship is present at even very low levels of ozone. One possible mechanism by which ozone could act indoors at low levels is suggested by a study in which indoor levels of several chemicals such as aldehydes were highly correlated with outdoor ozone concentration due to reaction of ozone with indoor air pollutants. Biological mechanisms responsible for the ozone-mortality relationship are largely unknown although effects of ozone on the autonomic control of the cardiovascular system, on coagulation mechanisms, and on vasoactive substances in the blood are being actively investigated.
What are the other potential effects of short-term ozone exposure?
There is consistent epidemiologic evidence that ambient ozone levels are associated with other markers of respiratory morbidity, particularly during the warm season. In general, studies have reported positive relationships between short-term ozone concentrations and hospital admissions and emergency room visits for respiratory causes (e.g. New Figure xx with the range of risk estimates plus the existing figure 5. I think current figure 5 makes the point as simply as possible). Although not all studies have found significant effects, risk estimates for the majority of studies are greater than zero. The evidence indicates that some of the increase in respiratory morbidity is due to exacerbations of asthma which will be discussed in the next section. Because of the small numbers of daily admissions for other subcategories of respiratory disease the effects of ozone on chronic obstructive pulmonary disease exacerbations and respiratory infections are not clear. Although it has not been fully evaluated, it is likely that those at most risk of serious respiratory morbidity are those with underlying respiratory disease such as asthma or COPD. A relationship has also been observed between ozone and school absences in two studies. However, in one case the absences were related to a measure of longer-term exposure, and in the other case absences were not limited to those due to illness. Although these results are suggestive, more research needs to be done before reaching a conclusion.
Ozone has been associated with daily hospitalizations for cardiovascular disease in some studies but not consistently. A number of studies have explored the relationships between ozone and various other aspects of cardiovascular pathophysiology including heart rate variability, acute myocardial infarction, and tachyarrhythmias in those with implanted cardiac devices. Although some data are suggestive of a relationship, the results at this time do not fully substantiate a relationship between ozone exposure and adverse cardiovascular events.
At what exposure levels are effects observed?
The lowest concentration at which effects are observed depends upon the level of activity, the duration of exposure, and the sensitivity of each individual to ozone. Although this is almost certainly true for all effects of ozone, levels that cause effects have been best characterized for symptom and lung function changes that can be studied under controlled exposure conditions. For example, a young adult of average sensitivity playing an active sport such as soccer or full court basketball outdoors for 2 hours would be expected to experience small lung function and symptom effects following exposure to 120 parts per billion (ppb) ozone. An average outdoor laborer doing heavy work might experience similar small effects following an 8-hour exposure to 60 to 70 ppb ozone and lung injury and inflammation following an 8-hour exposure to 80 ppb ozone. More sensitive individuals will experience such effects at lower concentrations while less sensitive individuals will experience these effects only at higher concentrations. Individuals who participate in less strenuous activity (e.g. gardening or delivering the mail) for shorter durations will still experience these effects but not until they are exposed to higher concentrations than if they were doing longer, more intense exercise. Children without asthma experience lung function decrements similar to those of young adults, but do not report respiratory symptoms at the lowest ozone concentrations. It is not clear whether this is the result of reduced sensitivity with regard to symptoms or whether children are less likely to recognize and report mild symptoms. Although the results vary somewhat, several field studies suggest that the lung function of highly active asthmatic and ozone sensitive children and the exercise performance of endurance athletes may be affected on days when the 8-hour maximum ozone concentration is less than 80 ppb ozone. Field studies of agricultural workers and hikers suggest that lung function changes may be associated with prolonged ozone exposures at lower levels than those observed in chamber studies.
For effects measured in some other types of observational studies, the lowest levels at which effects are expected to occur are more difficult to identify for a number of reasons. Effects of ozone on daily mortality have been detected even when study days are restricted to those with a 24-h average ozone concentration below 60 ppb (approximately equivalent to an 8-h average below 90 ppb). In one study hospital admissions for respiratory causes appear to follow a linear relationship down to background levels. ( Figure 5). Although controversial, limited exposure-response modeling suggests that if a population threshold for these ozone effects exists, it is likely near the lower limit of ambient ozone concentrations in the United States. Emergency room data from one study indicate that asthma attacks in the most sensitive population (e.g., children with asthma or reactive airway disease) increase following days on which the 1-hour maximum ozone concentrations exceeded 110 ppb (approximately equivalent to an 8-h average of 82 ppb) . (White et al., 1994) Another study observed increased emergency room visits for asthma on days following those when 7-hour averages exceeded 60 ppb compared to those with lower ozone concentrations. (Weisel et. al., 1995).
What are the effects of recurrent or long-term exposure to ozone?
One of the major unanswered questions about the health effects of ozone is whether repeated episodes of damage, inflammation, and repair induced by years of recurrent short-term ozone exposures result in adverse health effects beyond the acute effects themselves.
Daily ozone exposure for a period of 4 days results in an attenuation of some of the acute, neurally-mediated effects (e.g., lung function changes and symptoms) for subsequent exposures occurring within 1 to 2 weeks. Some health experts have, therefore, suggested that individuals living in high ozone areas may be protected from any harmful effects of long-term ozone exposure. Others suggest, however, that the attenuation of the ozone-induced tendency to take rapid and shallow breaths may blunt a protective mechanism, resulting in greater delivery and deposition of ozone deeper in the respiratory tract.
Studies including bronchoalveolar lavage and bronchial mucosal biopsies indicate that, unlike the neurally-mediated lung function changes, the processes of airway injury, inflammation, and repair continue to occur during repeated exposure. After either 4 or 5 days of exposure, markers of cell injury and increased epithelial permeability remain elevated, and an increase in airway mucosal PMNs, which was not present following a single exposure, has been noted. Also, unlike the neurally-mediated effects, small airway function has been observed to remain depressed over the course of exposures and is thought to be related to the ongoing inflammation.
Studies of laboratory animals have consistently demonstrated that long-term exposure to ozone concentrations above ambient levels results in persistent morphological changes that could be a marker of chronic respiratory disease. Exposed animals experience mucous cell metaplasia and epithelial cell hyperplasia in the upper airway as well as structural changes in the lower airway including an increase in fibrous tissue in the basement membrane area and a remodeling of the distal conducting airways. In addition to airway remodeling and basement membrane changes, concurrent long-term exposure of very young primates to ozone and house dust mite allergen has been observed to result in changes in the innervation of the airways as well as an accumulation of eosinophils in the distal airways suggesting induction of an allergic phenotype. Other studies indicate that sensitization of animals to antigen occurs more easily during ongoing ozone exposures. Although there is little evidence that long-term exposure in animals results in substantial alterations of traditional measures of airway function, these morphological findings suggest that long-term ozone exposure might play a role in the development or progression of chronic lung disease and/or asthma in humans.
The epidemiologic evidence is inconclusive with regard to whether long-term exposure of humans is related to chronic respiratory health effects in humans. Several cross-sectional studies have found that young adults who spent their childhoods in locales with high ozone concentrations had lower measures of lung function than those from locales with lower ozone. Similar results have not been observed, however, in a recent well-conducted longitudinal study of lung function in children or in other cross-sectional studies. Two longitudinal studies have observed associations between development of asthma and long-term ozone concentrations in subgroups of the population. These findings have not been confirmed in other longitudinal or cross-sectional studies, but they are consistent with the animial toxicological literature. Part of the difficulty in evaluating such associations has been the paucity of longitudinal epidemiologic studies specifically designed to evaluate respiratory health in samples with differing ozone exposures.. The mobility of the population as well as the inability to precisely estimate exposure to ozone and other potential confounders over a period of many years degrades the power of, and leads to bias in, both longitudinal and cross-sectional studies.
In spite of the inconclusive nature of the epidemiologic literature, the repeated cycles of damage, inflammation, and repair in humans and the morphological findings from the animal toxicological studies suggest that it would be prudent to avoid repeated short-term exposures, particularly in young children, until more is known about the effects of long-term ozone exposure.
| Review Key Points |
 |
 |
|
 Figure 2: Ozone is highly reactive in the respiratory tract.
When breathed into the airways, ozone interacts with proteins and lipids
on the surface of cells or present in the lung lining fluid, which decreases
in depth from 10 µm in the large airways to 0.2 µm in the alveolar
region. Epithelial cells lining the respiratory tract are the main target
of ozone and its products. These cells become injured and leak intracellular
enzymes such as lactate dehydrogenase into the airway lumen, as well
as plasma components. Epithelial cells also release a variety of inflammatory
mediators that can attract PMNs into the lung, activate alveolar macrophages,
and initiate a train of events leading to lung inflammation. Antioxidants
present in cells and lining fluid may protect the epithelial barrier
against damage by ozone or its reaction products.
Figure 2: Ozone is highly reactive in the respiratory tract.
When breathed into the airways, ozone interacts with proteins and lipids
on the surface of cells or present in the lung lining fluid, which decreases
in depth from 10 µm in the large airways to 0.2 µm in the alveolar
region. Epithelial cells lining the respiratory tract are the main target
of ozone and its products. These cells become injured and leak intracellular
enzymes such as lactate dehydrogenase into the airway lumen, as well
as plasma components. Epithelial cells also release a variety of inflammatory
mediators that can attract PMNs into the lung, activate alveolar macrophages,
and initiate a train of events leading to lung inflammation. Antioxidants
present in cells and lining fluid may protect the epithelial barrier
against damage by ozone or its reaction products.  Figure 3: Ozone induces neurally mediated responses in the bronchial
airways.
Figure 3: Ozone induces neurally mediated responses in the bronchial
airways.
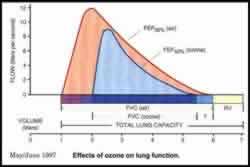 Figure 4: Effects of ozone on lung function. Ozone reduces the maximal inspiratory position (at the left of the curves) and may slightly increase the residual volume (at the right). Reduction in maximum inspiration reduces forced vital capacity (FVC), and this causes a reduction in expiratory flow measurements, such as flow at 50% of FVC expired (FEF50%). Because ozone causes only a small change in resistance, the relationship between flow and volume is not changed to a large extent.
Figure 4: Effects of ozone on lung function. Ozone reduces the maximal inspiratory position (at the left of the curves) and may slightly increase the residual volume (at the right). Reduction in maximum inspiration reduces forced vital capacity (FVC), and this causes a reduction in expiratory flow measurements, such as flow at 50% of FVC expired (FEF50%). Because ozone causes only a small change in resistance, the relationship between flow and volume is not changed to a large extent.  Figure 5: The number of emergency or urgent daily respiratory admissions
to acute care hospitals is related to estimated ozone exposure.
Respiratory admission rates to 168 hospitals in Ontario, Canada during the period 1983 through 1988 are plotted against deciles of the daily 1-hour maximum ozone concentration, lagged by 1 day. Admission rates were adjusted for seasonal patterns, day-of-week effects, and hospital effects. Ozone displayed a positive and statistically significant association with respiratory admissions for 91% of the hospitals during the Spring through Fall seasons, but not during the Winter months of December to March when ozone levels were low. Source: Burnett et al., 1994; U.S. EPA, 1996
Figure 5: The number of emergency or urgent daily respiratory admissions
to acute care hospitals is related to estimated ozone exposure.
Respiratory admission rates to 168 hospitals in Ontario, Canada during the period 1983 through 1988 are plotted against deciles of the daily 1-hour maximum ozone concentration, lagged by 1 day. Admission rates were adjusted for seasonal patterns, day-of-week effects, and hospital effects. Ozone displayed a positive and statistically significant association with respiratory admissions for 91% of the hospitals during the Spring through Fall seasons, but not during the Winter months of December to March when ozone levels were low. Source: Burnett et al., 1994; U.S. EPA, 1996